GASTROENTERITIS
1. Introduction
Gastroenteritis is a medical condition characterized by
inflammation of the gastrointestinal tract that involves both the stomach and
the small intestine resulting in some combination of diarrhoea, vomiting, and
abdominal pain and cramping.
Gastroenteritis is referred to as gastro, stomach bug, and
stomach virus. It has also been called stomach flu and gastric flu.
Most cases in children are caused by rotaviruses.
In adults, noroviruses and Campylobacter are more common.
Less common causes include other bacteria (or their toxins)
and parasites.
Transmission may occur due to consumption of improperly
prepared foods or contaminated water or via close contact with individuals who
are infectious.
2. Groups of pathogens that causes Gastroenteritis
a.
Rotavirus is the most common cause of severe diarrhoea
among infants and young children.
b.
Noroviruses are the most common cause of viral
gastroenteritis in humans . The viruses are transmitted by fecally-contaminated
food or water; by person-to-person contact; and via aerosolization of the virus
and subsequent contamination of surfaces
c.
Campylobacter is a genus of bacteria that are
Gram-negative, spiral, and microaerophilic . The sites of tissue injury include
the jejunum, the ileum, and the colon. Gastrointestinal perforation is a rare
complication of ileal infection.
3. 3. Signs and Symptoms
Gastroenteritis typically involves both diarrhea
and vomiting .
Abdominal cramping may also be present .
Signs and symptoms usually begin 12–72 hours
after contracting the infectious agent.
Some viral causes may also be associated with
fever, fatigue, headache, and muscle pain .
If the stool is bloody, the cause is less likely to
be viral and more likely to be bacterial .
Dehydration is a common complication of diarrhea
and a child with a significant degree of dehydration may have a prolonged
capillary refill, poor skin turgor, and abnormal breathing.
Repeat
infections are typically seen in areas with poor sanitation, and malnutrition,
stunted growth, and long-term cognitive delays can result .
Low grade fever (100 F)
Loss of appetite .
Loss of important electrolytes.
This may be signaled by little or no urine, extreme
thirst, lack of tears, and dry mouth.
4. Causes
1.Viral
a.
Rotavirus, norovirus, adenovirus, and astrovirus
are known to cause viral gastroenteritis. Rotavirus is the most common cause of
gastroenteritis in children. Rotavirus is a less common cause in adults due to
acquired immunity.
b.
Norovirus is the leading cause of gastroenteritis
among adults. Norovirus is the cause of about 10% of cases in children.
2.Parasitic
c.
E. histolytica, is pathogenic; infection can
can lead to amoebic dysentery or amoebic liver abscess.
d.
Giardia lives inside the intestines of
infected humans or other animals. The Giardia parasite originates from
contaminated items and surfaces that have been tainted by the feces of an
infected animal.
e.
Cryptosporidium is the organism most commonly
isolated in HIV-positive patients presenting with diarrhea and can cause
gastrointestinal illness with diarrhea in humans.
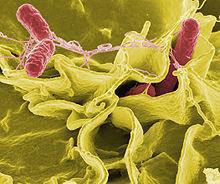
3. Bacterial
Campylobacter jejuni is the primary cause of bacterial
gastroenteritis. Bacteria are the cause in about 15% of cases, with the most
common types being Escherichia coli, Salmonella, Shigella,
and Campylobacter species.
Toxigenic Clostridium difficile is an
important cause of diarrhea that occurs more often in the elderly.
“Traveler's diarrhea" is usually a
type of bacterial gastroenteritis.
5.Transmission
Transmission may occur via consumption of contaminated water, or when
people share personal objects.Bottle-feeding of babies with improperly sanitized bottles is a
significant cause on a global scale.
Transmission rates are also related to poor hygiene, and in those with
pre-existing poor nutritional status.
Some agents (such as Shigella) only occur in primates(a mammal of
the order Primates, which contains prosimians and simians) , others may occur
in a wide variety of animals
Diangnosis
Gastroenteritis is typically diagnosed clinically, based on a person's signs
and symptoms.
Stool cultures should be performed in those with blood in the stool,
those who might have been exposed to food poisoning, and those who have
recently traveled to the developing world.
Diagnostic testing may also be done for surveillance. As hypoglycemia
occurs in approximately 10% of infants and young children, measuring serum
glucose in this population is recommended.
Electrolytes and kidney function should also be checked when there is a
concern about severe dehydration.
6. Prevention
Measures
Gastroenteritis is usually an acute and self-limiting disease that does
not require medication. The preferred treatment in those with mild to moderate
dehydration is oral rehydration therapy (ORT).
Metoclopramide and ondansetron, however, may be helpful in
some children.
Butylscopolamine is useful in treating abdominal pain .
Rehydration
The primary treatment of gastroenteritis in both children and
adults is rehydration.
Drinks especially high in simple sugars, are not recommended
in children under 5 years of age as they may increase diarrhea.
Plain water may be used if more specific and effective ORT
preparations are unavailable .
A nasogastric tube can be used in young children to administer fluids if
warranted.