ENTERIC
BACTERIA: SALMONELLOSIS
Introduction
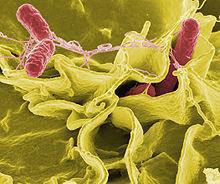
Salmonella is a gram
negative rods genus belonging to the Enterobacteriaceae family. Within 2
species, Salmonella bongori and Samonella enterica, over 2500 different serotypes
or serovars have been identified to date.
•Salmonella
is a ubiquitous and hardy bacteria that can survive several weeks in a dry
environment and several months in water.
Salmonella
Species
Zoonotic infection
Gram
negative intracellular organism
Family:
Enterobactericeae
Genus:
Salmonella
•2
Species: S. enterica (choleraesuis) 6 subspecies and S. bongori
– S. enterica subsp. enterica (I) Warm-blooded
animals
– S. enterica subsp. salmae (II) Cold-blooded animal
– S. enterica subsp. arizonae (IIIa) Cold-blooded
animal
– S. enterica subsp. diasonae (IIIb) Cold-blooded
animal
– S. enterica subsp. houtenae (IV) Cold-blooded
animal
– S. enterica subsp. Indica (VI) Cold-blooded animal
– S.
bongori (V) Cold-blooded animal
Salmonellosis
•Enteric
fever (systemic illness with fever and abdominal symptoms)
– Typhoid fever: Salmonella Typhi
– Paratyphoid fever: Salmonella Paratyphi A, B, or C
•Non-typhoidal
salmonellosis: other Salmonella serotypes
– GASTROENTERITIS
– BACTEREMIA & VASCULAR INFECTION
– SALMONELLOSIS & HIV INFECTION
– LOCALIZED INFECTION
– CARRIER
STATE
Epidemiology
The burden of foodborne
diseases is substantial: every year almost 1 in 10 people fall ill and 33
million of healthy life years are lost.
•
Foodborne diseases can be severe, especially for young children.
•Diarrhoeal
diseases are the most common illnesses resulting from unsafe food, 550 million people falling ill each year, including 220 million children under the age of 5 years.
• Salmonella
is 1 of the 4 key global causes of
diarrhoeal diseases.
S. Typhi and S. Paratyphi: reservoir only in human
• Typhoid fever is decreasing in incidence
• Non-typhoidal infection is increasing
• Rare typhoid fever in the Northeast of Thailand
• Risk factors: eat contaminated food, i.e.- water,
raw
vegetable, ice cream.
TRANSMISSION
•FOOD, WARTER BORNE
•FECAL-ORAL
ROUTE
Common Source of infection
•Contaminated food
•Poor hygiene kitchen
•Excretions from either sick or carrier of human
and animal
•Polluted surface water and standing water
•Unwashed fruit
•Un-hygienically
thawed fowl
FACTORS DETERMINE DISEASE DEVELOPING
•Number of organism 10,000,000-10,000,000,000
•Virulencity
•Host factors
HOST FACTORS
•High gastric pH: antacid, achlohydria
•Immunocompromise (CMIR)
–HIV
–Steroid (SLE)
–Malignancy
–Malnutrition
–Immunosuppressive therapy
–Extreme age
•Virulencity
•Host factors
HOST FACTORS
•High gastric pH: antacid, achlohydria
•Immunocompromise (CMIR)
–HIV
–Steroid (SLE)
–Malignancy
–Malnutrition
–Immunosuppressive therapy
–Extreme age
Pathophysiology
SIGNS & SYMPTOMS ENTERIC FEVER
•FEVER
•ABDOMINAL SYMPTOMS
•HEPATOMEGALY 50%
•SPLENOMEGALY 50%
•ROSE SPOT 30%
•CERVICAL LYMPHADENOPATHY
•NEUROLOGICAL SYMPOTOMS
•RALES
•ABDOMINAL SYMPTOMS
•HEPATOMEGALY 50%
•SPLENOMEGALY 50%
•ROSE SPOT 30%
•CERVICAL LYMPHADENOPATHY
•NEUROLOGICAL SYMPOTOMS
•RALES
CLINICAL OF ENTERIC FEVER
•Insidious
onset
•Non specific constitutional symptoms
(malaise, myalgia, chills, headache, dizziness, cough)
•GI symptoms (Anorexia/Nausea/ Vomitting/ diarrhea /abdominal cramps)
•Fever remittent
•Respiratory symptom
•SECOND AND THIRD WEEK
–PERSISTENT FEVER
–SYMPTOMS CONTINUE
•FORTH WEEK
–SPONTANEOUS REMISSION
•Non specific constitutional symptoms
(malaise, myalgia, chills, headache, dizziness, cough)
•GI symptoms (Anorexia/Nausea/ Vomitting/ diarrhea /abdominal cramps)
•Fever remittent
•Respiratory symptom
•SECOND AND THIRD WEEK
–PERSISTENT FEVER
–SYMPTOMS CONTINUE
•FORTH WEEK
–SPONTANEOUS REMISSION
LABORATORY: Enteric fever
•CBC
: Anemia, thrombocytopenia
•Transient leukocytosis then normal to leukopenia, PMN predominant
•LFT: mild elevation of liver enzymes
•jaundice mild
•BUN Cr: normal
•UA: normal
•CXR: normal to non-specific
•Transient leukocytosis then normal to leukopenia, PMN predominant
•LFT: mild elevation of liver enzymes
•jaundice mild
•BUN Cr: normal
•UA: normal
•CXR: normal to non-specific
LABORATORY: Enteric fever
•Blood
culture
•Bone marrow culture 90%
•Stool, urine culture
•Duodenal content culture
•Serology : Widal test not reliable, insufficiently sensitive, specific, or rapid enough for clinical use
•Bone marrow culture 90%
•Stool, urine culture
•Duodenal content culture
•Serology : Widal test not reliable, insufficiently sensitive, specific, or rapid enough for clinical use
TREATMENT
•EFFECTTIVE
ATB
–FLUROLOQUINOLONE
–AMPICLLIN
–CHLORAMPHENICOL
–CO-TRIMOXAZOLE
–3rd
GENERATION CEPHALOSPORIN
•Uncomplicated
Typhoid Fever
–Ciprofloxacin
500mg BID 5-7Days
–Ofloxacin 400mg BID 5-7Days–Ceftriaxone 2g I.V daily 10-14 days
–Cefixime 200mg BID 7-14days
–Azithromycin 1g PO daily for 7 days
–Trimethoprim-sulfamethoxazole 160/800mg BID 7days
–Ofloxacin 400mg BID 5-7Days–Ceftriaxone 2g I.V daily 10-14 days
–Cefixime 200mg BID 7-14days
–Azithromycin 1g PO daily for 7 days
–Trimethoprim-sulfamethoxazole 160/800mg BID 7days
•Sever
complicated Typhoid Fever:
–Ampicillin 2g every 6 hrs for 14day
–Chloramphenicol 1.5 IV every 6hours 14-21days
–Ampicillin 2g every 6 hrs for 14day
–Chloramphenicol 1.5 IV every 6hours 14-21days











0 comments:
Post a Comment